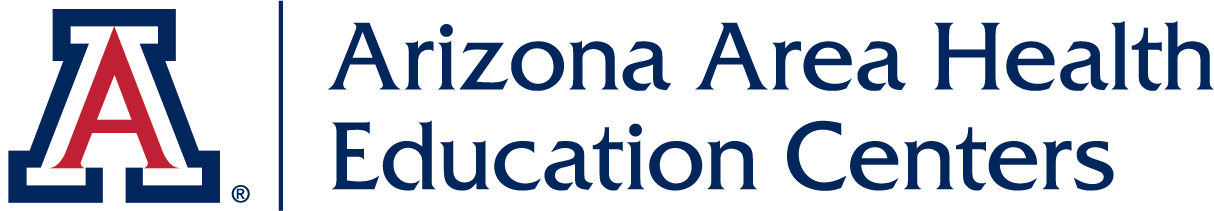
Many intractable health problems – including limited access to health services and disparities in health outcomes between rural and urban populations, economic and ethnic groups, employed and unemployed, insured and uninsured - have social determinants. A conceptual framework (Figure 1) of transformative, lifelong, community-engaged health professions learning effectively addresses the social determinants of health (SDOH). Cornerstones of the AHEC Scholars Program include experiential and collaborative learning, an integrated health professions curriculum, and continuing professional development.
Figure 1: AHEC Scholar Conceptual Model. Adapted from: National Academies of Sciences, Engineering, and Medicine. (2016). A framework for educating health professionals to address the social determinants of health. National Academies Press.
The AHEC Scholars Conceptual Learning Model is based on the National Academies of Science framework for lifelong learning. Progressive learning occurs in four phases over the two years of the program:
- Introduction to rural and medically underserved communities (MUCs) - rapidly familiarizes AHEC Scholars on core concepts, vocabulary, team-based learning, collaborative practice, and being a successful Scholar. Topics include social determinants of health, cultural competence, behavioral health integration, practice transformation, connecting communities and supporting health professionals, current and emerging health issues, and required learning activities.
- Rural and MUC immersion - involves direct engagement in the assigned AHEC Regional Center, including individual community members, families, and community organizations. Scholars experience the unique characteristics of communities served by Regional Centers. These provide engagement with communities and foster team-based, collaborative, interactive work to assess and work on problems identified. Scholars learn with each other and community partners, applying theoretical knowledge to assess their population of interest. Scholars spend time in their assigned communities and their team. Scholars remain with their cohort team and community over the two-year program.
- Integration - involves student teams working together on a hands-on scholarly project from their population of interest and assessment activities. The seminars and scholarly projects teach core competencies and sometimes influence practice location choice after graduation. Integration empowers Scholars to synthesize content, teaching, learning, and knowledge about rural and underserved areas. Outreach and community engagement prepare Scholars with practice-ready, team-based skills to effectively work in rural and medically underserved communities.
- Informed dissemination - teaches skills in presenting, data visualization, writing, and disseminating information, reports, and recommendations to lay and professional audiences.
The following tables summarizes the progressive pathway of the ASP:
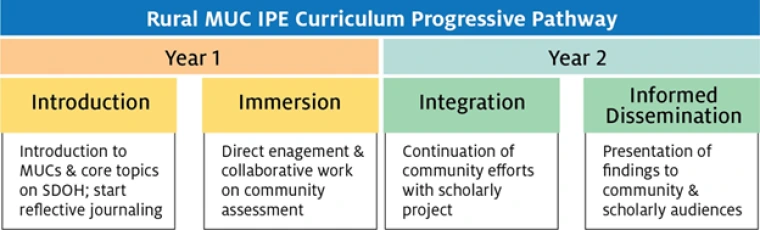
MUC: Medically Underserved Community; SDOH: Social Determinants of Health; IPE: Interprofessional Education